Your Pregnancy / Tō Hapūtanga - HE1420
On being pregnant and keeping healthy (avoiding alcohol, smoking and drugs), labour and giving birth, the first few weeks after the birth of your baby, and the roles and responsibilities of LMCs (Lead Maternity Carers).
The full resource:
A guide to pregnancy and childbirth in New Zealand
Table of Contents - Te Rārangi Kōrero
Being pregnant – Kua hapū
Choosing an LMC
Care you’re entitled to
Antenatal screening
Receiving care from a specialist
Other maternity services
Parental leave
Your developing baby – A brief overview
Twins
Keeping healthy in your pregnancy
Labour and birth – Te whakawhānau
Antenatal classes/childbirth education
Preparing for birth
The stages of labour
Variations in labour and birth
After the birth – I muri iho i te whānautanga
Postnatal care
Screening for your baby
Breastfeeding
Safe sleeping
Registering your baby’s birth
Start of your Well Child visits
Immunisation
Returning to work
Appendices
Further information for pregnant women
Choosing an LMC
Important contacts
Complaints
Being pregnant - Kua hapū
Choosing an LMC
Once you know that you are pregnant, you need to make several important decisions, such as finding a Lead Maternity Carer (LMC). Your LMC can be a midwife, a general practitioner (GP) or a specialist obstetrician. You may register with an LMC as soon as you become pregnant. You may also receive first trimester care (up until the 12th week of pregnancy) from a GP, even if they are not your LMC.
Phone 0800 MUM 2 BE (0800 686 223) to request a list of names and phone numbers of LMCs in your area. You can also look for ‘midwives’ in the yellow pages, or look on the Find Your Midwife website (www.findyourmidwife.co.nz). The information in the appendix Choosing an LMC lists a range of questions you can ask that may help you choose your LMC.
Once you have decided who your LMC will be, you will be asked to sign a form called Registration of Woman with LMC. Once you have registered with an LMC, your LMC is responsible for your maternity care throughout your pregnancy and until six weeks after the birth of your baby. Your baby’s care will then be transferred to your chosen Well Child provider, and your care will return to your usual GP. See Start of your Well Child visits for further information on this.
Contact your LMC with any questions about your pregnancy. From the time you register until your last mother and baby check-up, your LMC, or their backup, is available to help you with phone advice or a visit if necessary. Either your LMC or backup LMC will be available 24 hours a day, seven days a week (after hours contact for urgent care). You can choose to change your LMC at any time.
Care you’re entitled to
Maternity care is free for New Zealand citizens, women with permanent residency, those who have a work permit and are able to stay for two years, or those who are eligible in another way (the full set of criteria is on the Ministry of Health’s website). If you are not eligible but your partner is, your maternity-related services may be publicly funded. Babies born in New Zealand are eligible for free care if their mother is eligible for free maternity care. If you are not sure whether you are entitled to free maternity care, call freephone 0800 686 223.
Things your LMC or backup LMC will do:
- take responsibility for your care throughout your pregnancy, labour and the birth, and for you and your baby’s care until six weeks after your baby is born
- provide you with information to help you make choices about your care
- provide you with free maternity care if you are eligible (unless your LMC is a private obstetrician)
- refer you or your baby to a specialist if it becomes necessary
- develop a plan with you for your care, including your labour and the birth
- be with you during your labour and the birth (or visit when needed)
- visit you at the hospital and in your home between five and ten times after your baby is born (more if clinically needed) or arrange for a midwife to provide these visits if your LMC is a doctor
- refer you to your chosen Well Child provider at a time agreed by you. This will usually be between four and six weeks after the birth of your baby
- provide a written note to your GP before discharging you from their care.
Note that if you see a GP for your first trimester care and then register with another doctor or midwife to be your LMC, the GP should provide you with important health information to give to your LMC. This includes a written summary of your care and any health concerns, as well as copies of results for blood tests and screening from your first trimester.
Your LMC will see you regularly throughout your pregnancy. The LMC will palpate (feel) your abdomen to check your baby’s growth, position and heartbeat, take your blood pressure and explain to you what the results of these checks mean for your pregnancy. They will organise other tests to check on you and your baby. They will also explain how often you need to be seen during your pregnancy and whether these visits will be in your home or at a clinic, marae maternity clinic or hospital.
Your LMC will also discuss things with you such as:
- whether they will stay involved if you require specialist services
- their contact information for urgent situations
- what they will do to make sure your cultural or spiritual practices are observed or followed
- what education they will provide during pregnancy for labour and birth and for after the birth
- the situations when you will need referral to other midwifery, medical, social and diagnostic services
- smoking cessation
- screening for infectious diseases
- safety in your home.
Contact your LMC if you have concerns about your pregnancy. This may include bleeding, excessive vomiting, if you think your waters have broken, abdominal pain, reduced fetal movements or other illness or concerns.
Antenatal screening
During your pregnancy, you will be advised of screening for a number of conditions that may affect you or your baby. You will be provided with information to help you choose whether you would like to have this screening.
First antenatal blood screen
When you first see your LMC or GP during pregnancy you will be offered a first antenatal blood screen. This is to test for:
- your blood group and rhesus factor (If you are rhesus negative, ask your GP or LMC to explain what this means.)
- your haemoglobin (iron content in your blood)
- the presence of any antibodies that may be harmful to your baby
- whether you are immune to rubella
- whether you are a hepatitis B carrier
- whether you have syphilis
- whether you have HIV (see Antenatal HIV screening).
Antenatal HIV screening
In New Zealand, all pregnant women are offered antenatal HIV screening. If you have HIV, treatment can help keep both you and your baby well. (Diagnosis and appropriate treatment in pregnancy reduces the risk to the baby of getting the virus from 30 percent to less than 1 percent.)
Screening for HIV involves you having a blood test. Your LMC or GP will offer you the test at the same time as the first antenatal blood screen, usually during your first pregnancy visit.
The screening test for HIV is very reliable and picks up almost every woman with HIV. As with all screening tests, some women will get a positive screening result but will not have HIV. About one woman out of every 1000 who have the test will need to have a second blood test to confirm whether or not they have HIV. Your LMC or GP will discuss with you what the results may mean.
For more information, see the brochure HIV testing in pregnancy (available from your LMC or GP, or at www.healthed.govt.nz) or the National Screening Unit's website.
Antenatal screening for Down syndrome and other conditions
Your LMC or GP will advise you of the availability of antenatal screening for Down syndrome and other conditions. This screening is optional. Choosing whether to have this screening is an important decision. You need to have enough information to make the decision that is right for you. You do not have to have screening and testing if you do not want to.
Down syndrome is the most common condition indicated by this screening. Other, more rare conditions include Edwards syndrome (also called trisomy 18) and Patau syndrome (also called trisomy 13).
First trimester combined screening
This screening is offered if you are less than 14 weeks pregnant. It includes a blood test from you and measurements of your baby including nuchal translucency or NT taken from an ultrasound scan. The blood test is free; you may be charged for the scan. The laboratory combines the blood test and scan results with other information, such as your age and weight, to work out the chance of your baby having one of the screened conditions.
Second trimester maternal serum screening
This screening is offered if you are 14 to 20 weeks pregnant. It involves a blood test from you. This blood test is free. The laboratory combines the blood test results with other information, such as your age and weight, to work out the chance of your baby having one of the screened conditions.
Getting your screening results
Your results will be ready in about 7 to 10 days. Your LMC or GP will discuss your results with you and what they may mean for you. If there is an increased chance that your baby has one of the screened conditions, you will be offered a referral to a specialist. The specialist will discuss what your results mean and your options, including diagnostic testing.
Diagnostic testing
Diagnostic testing, through an amniocentesis or chorionic villous sampling (CVS), will tell you for sure whether your baby has Down syndrome or another screened condition. Diagnostic tests look at a sample of your baby’s cells. Diagnostic testing is your choice. For every 200 women who have diagnostic tests, one or two will have a miscarriage. For this reason, some women chose not to have diagnostic testing.
For more information, see the brochure Antenatal screening and testing for Down syndrome and other conditions (available from your LMC or GP, or at www.healthed.govt.nz) or the National Screening Unit's website.
Other antenatal blood tests
You will be offered a blood test around 26 to 28 weeks of pregnancy to screen for diabetes in pregnancy. This is called a polycose test. If your polycose level is high, you will be offered a glucose tolerance test that will confirm whether or not you have diabetes in pregnancy.
Information is available from your LMC or GP to help you decide whether to have these screening tests.
Receiving care from a specialist
If complications should arise during your pregnancy or labour, you will need to decide whether you want to use publicly funded hospital specialist services or a private specialist. In many places in New Zealand, only fully publicly funded hospital specialist services are available. (If your LMC thinks you should consult a specialist, they will discuss this with you.) In many cases in which a pregnant woman requires specialist services, their LMC will continue to provide the primary care that is part of the LMC role, but there are times when full transfer of care to a specialist is necessary. Before full transfer of care or responsibility for care is made, a discussion between you, your LMC and the specialist will take place. The ongoing role that your LMC now has in your care will be agreed between those involved. This includes you. If responsibility for your care transfers to the hospital specialist services after you have gone into labour, sometimes your LMC will continue to be available to support you, but this is not always possible.
Other maternity services
While most maternity care is publicly funded, there may be a charge if you choose to use some specialist or private services. For example:
- Private specialist services – care from a private obstetrician, paediatrician or anaesthetist, even where this care is provided within a public hospital. You will not have to pay for any care that you receive from hospital specialist services.
- Ultrasound scans are a specialist service, so radiologists practising in private may charge you a co-payment (a charge in addition to the fee paid to the radiologist by the government). Also, if you choose to have a scan and there is no medical reason for it, you will be charged for the service. If you are in the second or third trimester, any referral for an ultrasound scan must come from your LMC or an obstetrician.
- Laboratory tests – you may be charged a fee if you have any laboratory tests that are not routine during pregnancy.
- Ambulance service – if you use an ambulance service to go from the community or a primary maternity unit to a hospital, the ambulance service may charge you.
- Antenatal education – if you choose to go to an education class that is not funded by the government, it is likely there will be a charge.
- GP care – if you need to see your doctor during pregnancy for a problem that is unrelated to your pregnancy or for an existing medical problem that has become worse because of your pregnancy, you will be charged that doctor’s usual consultation fee. Some GPs providing first trimester or LMC care may not choose to receive Ministry funding, in which case you will need to pay for the care they provide.
In this case, you can choose to stay with your GP and pay for your care or find another provider who offers government-funded care.
Parental leave
You may be eligible for paid or unpaid parental leave, and some of this may be shared by your partner. Unpaid parental leave includes:
- maternity leave of 22 continuous weeks, which may start up to six weeks before your baby’s due date
- special leave of up to 10 days, which you can take before your maternity leave for reasons connected with pregnancy (eg, antenatal checks)
- Partner’s/paternity leave of either one or two weeks if your partner is an employee
- extended leave of up to 52 weeks, available if you have worked for your employer for more than 12 months leading up to the birth of your baby.
22 weeks of paid parental leave may be available to you if you meet the 6- or 12-month eligibility criteria for work leading up to the birth of your baby. You may transfer all or part of your paid parental leave to your partner as long as they are also eligible.
For further information about whether you are eligible for parental leave and how to apply for it, freephone the Department of Labour 0800 800 863.
Your developing baby – A brief overview
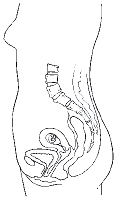
6–7 weeks
At seven weeks, the baby is about 8 mm long from head to bottom. The brain is developing, and the heart is beginning to beat. Physical features, such as the ears, eyes, arms and legs, are also developing.
8–9 weeks
At nine weeks, the baby is about 17 mm long from head to bottom. The face is slowly forming, with the eyes becoming more obvious.There is a mouth and tongue. Hands and feet, with ridges where the fingers and toes will be, are also beginning to develop.
10–14 weeks
Just 12 weeks after conception, the baby is fully formed. It has all its organs, muscles, limbs and bones. From now on, it will grow and mature. The baby is already moving about, but the movements cannot yet be felt. First-time mothers tend to feel the baby first move at about 20 weeks, while for second-time mothers, the first movements are felt at about 16 weeks.
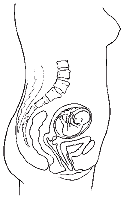
24 weeks

At 24 weeks, the baby is about 30 cm long and weights 0.6 kg. The baby's skin is thicker and less see-through (transparent), but remains wrinkled because there is no fat underneath. The baby is moving strongly and the eyelids are now separated. Baby starts practising breathing and swallowing movements.
28 weeks
At 28 weeks, the baby is over 38 cm long and is about 0.9 kg in weight. The baby’s skin begins to develop a white greasy covering called vernix, which waterproofs the skin. The baby’s movements can easily be felt at this stage.
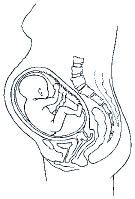
40 weeks
At 40 weeks, the baby is 50 cm long and weighs over 3 kg. Over the past four months, the baby has fully developed and the lungs have matured, ready for birth.
Other information about the development of your baby is available in resources such as The New Zealand Pregnancy Book by Sue Pullon and Cheryl Benn.
Twins
Identical twins develop from one fertilised egg splitting into two separate cells. They therefore have the same genes, are the same sex and look very alike.
Non-identical twins result from two eggs being fertilised at the same time and are more common than identical twins.


Keeping healthy in your pregnancy
Keeping healthy throughout your pregnancy includes eating healthy food, getting exercise, getting enough rest, preventing the spread of infection, not smoking or drinking alcohol, and not taking recreational drugs. It also includes maintaining your cultural, spiritual and emotional wellbeing.
See also Further information for pregnant women for details of pamphlets that contain information for women who are pregnant or who have just had a baby.
Taking care with medicines
Some medicines can harm the developing baby. Only take those medicines that have been recommended by your midwife or your doctor. Always check with them or your pharmacist before taking anything else. X-rays and some local and general anaesthetics (including dental X-rays and anaesthetics) are best avoided during pregnancy.
Smoking
Smoking during pregnancy affects the baby’s growth and will mean more likelihood of health problems such as:
- a lower birthweight that could be harmful
- an increased risk of cot death, pneumonia, asthma or glue ear
- a risk of miscarrying or having a stillborn baby.
There are programmes available to help pregnant women quit or reduce smoking. There is also information available on how to quit smoking. You can call the Quitline (Quit–Me Mutu) on 0800 778 778.
Alcohol
There is no known safe level of alcohol use during pregnancy. If you think you are pregnant or know you are pregnant, it is safer to avoid alcohol altogether.
When you are pregnant, alcohol that you drink is carried by your bloodstream through the placenta to your baby. Drinking alcohol during pregnancy can cause brain damage to your baby, and that damage is permanent. This damage is called Fetal Alcohol Syndrome (FAS) or Fetal Alcohol Effects or (FAE).
Drinking alcohol may harm your unborn baby because:
- there is a greater likelihood of miscarriage, stillbirth and premature birth
- babies may be born with intellectual disabilities or physical defects
- slower development may become obvious later in childhood, and the child may have poor co-ordination and learning and behavioural problems, including hyperactivity.
After the birth of your baby, some of any alcohol you drink will pass into your breast milk.
Cannabis and/or other recreational drugs
Using alcohol and/or other recreational drugs such as cannabis can cause special problems to the mother and baby, possibly causing premature birth or a low birthweight. Other drugs such as narcotics like heroin may cause the baby to be born drug-dependent and suffer from withdrawal symptoms. Drug-dependent babies will need expert management if they are to survive.
Diet
Eating well and doing moderate physical activity during pregnancy are important for you and your baby. Nutritional needs are higher when you are pregnant. Meeting these needs helps protect the long-term health of both you and your baby. It is important to eat a variety of healthy foods every day from each of the four main food groups:
- vegetables and fruit
- breads and cereals (wholegrain is best)
- milk and milk products (reduced- or low-fat milk is best)
- lean meat, chicken, seafood, eggs, legumes, nuts and seeds.
Drink plenty of fluids every day.
The only dietary supplements recommended for all pregnant women are folic acid and iodine. Folic acid is a vitamin that is needed for the formation of blood cells and new tissue. During pregnancy, your need for folic acid is higher. Lack of folic acid has been linked with neural tube birth defects, such as spina bifida. The risk of having a child with these birth defects is low but can be reduced by taking a folic acid tablet. Iodie is essential for normal growth and development including brain development. It is particularly important for the baby. Subsidised (reduced cost) folic acid and iodine tablets are available for all women. Discuss them with your LMC.
Some foods should be avoided because of the risk of catching listeriosis. Listeria is a common bacterium that can cause food-related illness. In pregnant women, this illness can cause miscarriage and stillbirth or it can cause infection in your baby. You can reduce your risk from listeria by avoiding certain foods and by using safe food practices. For more information on safe food practices, read the pamphlet Avoiding Listeria (available at www.healthed.govt.nz) and Food Safety in Pregnancy (available at www.mpi.govt.nz/food-safety/food-safety-forconsumers/food-and-pregnancy/).
The list of avoidable foods changes regularly. For an up-to-date list, refer to the MPI website or phone 0800 693 721. Examples of foods to avoid eating are:
- uncooked, smoked or ready-to-eat fish or seafood, including oysters, smoked ready-to-eat fish, sashimi or sushi*
- paté, hummus-based dips and spreads
- ham and all other chilled pre-cooked meat products including chicken, and fermented or dried sausages such as salami*
- pre-prepared or stored salads (including fruit salads) and coleslaws
- raw (unpasteurised) milk and any food that contains unpasteurised milk*
- soft-serve ice creams
- soft, semi-soft, or surface-ripened soft cheese (such as brie, camembert, feta, ricotta, and roquefort)*.
* Note that these foods are safe to eat if heated thoroughly until piping hot, that is, above 70 degrees Celsius.
Infections
Some infections during pregnancy can cause harm to your baby. If you are in contact with someone who has an infectious illness or you are not sure about symptoms, information is available to help you make any decisions about what you should do. Some of these infections include:
- rubella (German measles)
- toxoplasmosis – an infection that pregnant women can get from cat faeces and that can pass through the placenta to the baby
- human immunodeficiency virus (HIV)
- hepatitis B
- hepatitis C
- tuberculosis
- herpes.
A range of other infections, such as urinary tract infections, thrush, streptococcus B (strep B), chicken pox (varicella), and sexually transmitted infections (such as chlamydia or gonorrhoea) may also cause harm to you or your baby. If you come into contact with any of these infections, talk to your LMC.
Labour and birth - Te whakawhānau
Antenatal classes/childbirth education
Antenatal classes/childbirth education (also called pregnancy and parenting education) gives pregnant women, their partners, support people and families/whānau the opportunity to:
- learn more about what will happen to them and the care they are likely to receive during labour and the birth
- develop strategies to get through labour
- understand what happens after their baby is born
- meet other parents-to-be.
Preparing for birth
Every birth is different, and babies vary in when they arrive and how long they take to do so. Your LMC can answer any questions you might have about your labour and the birth and how you should prepare.
Your LMC will provide information to help you develop a birth plan:
- where to have your baby
- who you want to be with you
- what sort of environment you want and what position you may want to be in for giving birth
- choices for monitoring your labour, interventions that may be needed and treatment for things that don’t go well
- how to get breastfeeding started
- how long to stay in the hospital (if you go there) and plans for going home
- handling of placenta/whenua according to your wishes and culture
- support options for you after the birth and risk factors for postnatal depression.
Think about who you would like to support you at your baby’s birth. You may wish to have only your partner with you, or you may like other members of your family/whānau. You may have special cultural or spiritual practices that you wish to have for labour and at the birth, such as prayers/karakia.
Māori may wish the placenta/whenua to be kept and returned to them according to Māori tikanga and kaupapa. Other women may choose this too. Make this and any other preferences known to your LMC.
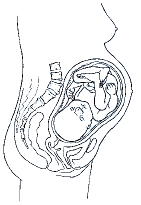
The stages of labour
 There are three main stages in labour. The time taken for each stage will vary from woman to woman. In the first stage the cervix opens, in the second stage the baby is pushed down through the vagina and is born, and in the third stage the placenta/whenua comes away from the wall of the uterus and is pushed out through the vagina.
There are three main stages in labour. The time taken for each stage will vary from woman to woman. In the first stage the cervix opens, in the second stage the baby is pushed down through the vagina and is born, and in the third stage the placenta/whenua comes away from the wall of the uterus and is pushed out through the vagina.
 The membrane that holds the amniotic fluid and your baby (often called ‘the waters’) can break at any time. Often this happens near the end of the first stage or at the beginning of the second stage of labour. Sometimes the waters are deliberately broken to help get labour started.
The membrane that holds the amniotic fluid and your baby (often called ‘the waters’) can break at any time. Often this happens near the end of the first stage or at the beginning of the second stage of labour. Sometimes the waters are deliberately broken to help get labour started.
 When you think you are in labour, tell your LMC. They will then advise you what to do next. Your LMC may visit and assess you in your home or meet you at the maternity hospital, or they make some other suggestion(s).
When you think you are in labour, tell your LMC. They will then advise you what to do next. Your LMC may visit and assess you in your home or meet you at the maternity hospital, or they make some other suggestion(s).
Variations in labour and birth
 No two births are the same.
No two births are the same.
You need to think about what pain relief you want during labour and the birth. Some strategies, such as relaxation and breathing techniques, keeping upright and mobile, a warm bath or shower, a birthing pool or a TENS machine, can be helpful. Medicines/rongoā, massage/mirimiri and prayer/karakia can also be helpful, as can homeopathy or aromatherapy. As you prepare for labour and the birth, discuss with your LMC any questions you have about relieving pain in labour through these strategies.
However, you may need extra help at your baby’s birth.
Medical pain relief
Gas, injections of drugs, or epidural or spinal anaesthetics can be used if necessary, although other methods should be tried first. It is important to note that all drugs pass through the umbilical cord to the baby up until the time the cord is cut, so only necessary drugs should be used. Some forms of medical pain relief increase the likelihood of other medical interventions.
Induction/augmentation of labour
Induction is when labour is started artificially because of risk to the mother or baby if the pregnancy went on any longer. Induction can be done by using the following:
- placing a medicated gel close to the cervix
- breaking the membrane that holds the amniotic fluid and your baby (‘the waters’)
- using intravenous synthetic hormones to cause the uterus to contract.
Inductions are likely to lead to increased intervention, such as a ventouse or forceps birth or a caesarean section.
Augmentation (assisting a labour that has already commenced) can be done by using the following:
- breaking the membrane that holds the amniotic fluid and your baby
- a hormone drip to strengthen the contractions.
Ventouse or forceps birth
Ventouse or forceps may be used to help deliver your baby. A ventouse is a suction cap that is placed on the baby’s head and, through firm pulling and you pushing, helps the baby to be born. The same method is used for a forceps birth, with the forceps being placed around the baby’s head. An episiotomy may be done for a ventouse or forceps birth. An episiotomy is when the perineum (area round the vaginal opening) is cut to make the opening bigger. Stitches are needed afterwards.
Caesarean section
A caesarean section is the removal of the baby from the uterus by surgery. This should only be done when there are medical reasons for it. An epidural or spinal anaesthetic is generally given. A general anaesthetic may be used when an emergency caesarean section is needed. After the operation, stitches or clips are used to seal the wound. These either dissolve or are removed about five to eight days later.
After the birth - I muri iho i te whānautanga
The postnatal period is the time for recovering from the birth and getting to know your baby. It is also a time for eating well, drinking lots of water, resting with your baby and getting support from your family/ whānau. It takes about six weeks for your body to return to its pre-pregnant state.
Postnatal care
You and your baby are entitled to six weeks of postnatal care by your LMC. Your baby will be checked by your LMC at each visit and given at least three more comprehensive examinations as well:
- within 24 hours of birth
- within seven days
- before being transferred to your chosen Well Child provider (ie, the health professional who will provide health care for your baby).
At your baby’s first examination, within 24 hours of birth, your LMC will check that your baby is feeding properly. Babies generally wake three to four hourly for feeding, although more frequently in the first days after birth (referred to as cluster feeding).
Vitamin K can be given to babies soon after birth to prevent the development of bleeding due to low vitamin K levels. This condition can be serious. Vitamin K can be provided by injection or by mouth. If given by mouth, three doses are required – at birth, one week and six weeks. It is important to get information from your LMC before your baby is born so that you can make an informed decision about whether or not you want your baby to have vitamin K.
Your LMC will also look for any potential health problems, such as jaundice. Newborn babies can have some mild jaundice about the third day after the birth. Jaundice gives the baby a yellow appearance and is easily remedied by frequent feeding. More severly jaundiced babies may need exposure to special light treatment, called phototherapy (treatment using blue light). This may involve the baby lying on special bed (bilibed) or having lights placed over the bassinet.
Hospital stay
If you have your baby in hospital, your LMC will visit you daily while you are in hospital unless they make special arrangements with the hospital staff. The length of your stay will depend on your clinical needs. The decision about when to leave will be made through discussions between you, your LMC, and the hospital staff.
In situations where your care has been transferred to the hospital specialist service, you will be transferred back to the care of your LMC when you no longer need the specialist service. Your LMC will explain what their role is, alongside that of the hospital specialist service, for the time you are in hospital.
Home visits
Once you have gone home, you can expect between five and 10 visits from your LMC or a midwife. You are entitled to at least five home visits unless you ask not to have them. If you had your baby in hospital, you will receive your first home visit within 24 hours of going home from hospital. The postnatal care you will receive from your LMC includes assistance with and advice about feeding and caring for your baby, as well as advice about caring for yourself, your nutritional needs and contraception.
Your LMC will refer your baby to your chosen Well Child provider. They will also refer you and your baby to your GP for ongoing care and the start of baby immunisations at 6 weeks of age.
Screening for your baby
Screening is an important way of identifying babies who are more likely than other babies to have a health issue. It is your choice whether your baby has screening. The Ministry of Health strongly recommends screening for your baby.
Newborn metabolic screening
The Newborn Metabolic Screening Programme detects rare but life-threatening metabolic disorders. This screening is a blood test and happens when babies are 48 hours old, or as soon as possible after this. Each year around 45 babies are found to have a metabolic disorder. Early diagnosis means that treatment can start quickly, before the baby becomes sick. Metabolic disorders are hard to find without screening.
Although these disorders cannot be cured, early treatment with medication or a special diet can help your baby stay well and prevent severe disability or even death. Metabolic disorders can occur in any family, even when there is no family history of disorders.
Your LMC will provide you with information about newborn metabolic screening (the heel prick test) before you consent for this test. Ask when to expect the results and consider whether you would like the leftover blood spots to be stored or returned to you after screening. Ask what these might be used for if stored.
For more information, see the brochure Your newborn baby’s blood test (available from your LMC or GP, or at www.healthed.govt.nz) or the National Screening Unit's website.
Newborn hearing screening
Parents or guardians of all babies born in New Zealand are offered the opportunity to have their baby’s hearing screened. This screening is designed to pick up moderate to profound hearing loss. If your baby can’t hear, it is hard for them to learn to speak, socialise and learn. Finding hearing loss early is important for your baby’s language, learning and social development.
Screening is usually done before you and your baby go home from the hospital. If your baby is not born in a hospital or not screened before you go home, screening may be offered at your local health clinic or hospital outpatients’ clinic. Screening should happen before your baby is one month of age. This is so that diagnostic testing can be completed by three months of age and, if a hearing loss is found, intervention can begin by six months of age.
You will be told the screening results straight away. Some babies need another screen because the earlier screening did not show a strong enough response in one or both ears. If this happens you will be offered a repeat screen, either before leaving the hospital or as an outpatient appointment. If your baby does not pass the screening, they will be referred to an audiologist for further testing. Most children who go to the audiologist will not have a hearing loss but need that additional testing to be sure.
Your LMC can provide you with more information about newborn hearing screening.
For more information, see the brochure Newborn Hearing Screening (available from your LMC or GP, or at www.healthed.govt.nz) or the National Screening Unit's website.
Breastfeeding
Breastfeeding is the best nutrition for your baby and has advantages for you too. To help make your breastfeeding experience positive, ask for information and advice early in your pregnancy. You can also talk to other mothers who have enjoyed breastfeeding their babies. Breastfeeding is a skill that needs to be learned. Some women experience no problems, whereas others need more help and support to get started and continue feeding. Having the practical support of your partner, family/whānau and friends is important.
Benefits of breastfeeding
The Ministry of Health recommends that all babies are fed only breast milk for the first six months of their life. This means no water, infant formula or fruit juices. After six months, you can slowly start your baby on solid foods and other fluids while you keep breastfeeding for one year or longer.
Breastfeeding is best for your baby because:
- it helps to develop a close bond between you and your baby
- breast milk is the only food that is exactly the right nutrition and temperature for your baby
- breast milk will help protect your baby from ear infections, gastroenteritis, respiratory infections and eczema.
Babies who are breastfed are less likely to have respiratory problems, coughs, colds or infections before they are one year old for which they may need to be admitted to hospital. Breastfeeding may also reduce the risk of cot death.
Breastfeeding is good for you because:
- you will recover from the birth faster
- it helps strengthen the natural bond between you and your baby
- you may lose weight gained during pregnancy faster
- you may be less likely to get some types of breast cancers
- you may be less likely to suffer from ovarian cancer, osteoporosis and hip fractures later in life.
Some things can help you breastfeed successfully. For example, a drug-free birth provides an excellent start. It is also important that you and your baby have skin-to-skin contact for at least the first hour after the birth and that you breastfeed your baby during this time. This develops a close bond and helps your body to begin producing breast milk. Your LMC can tell you about any support groups in your area, such as La Leche League, Parents Centre or Home Birth Association. There are also books and pamphlets available on breastfeeding.
Some mothers have health conditions or take medications that mean that they cannot breastfeed. If you are one of these mothers, discuss safe artificial feeding with your LMC.
If your new baby is not waking and feeding regularly (at least 3-4 hourly), contact your LMC because dehydration may be a problem or your baby may be unwell.
Safe sleeping
There are some important things you can do to reduce the risk of suffocation and sudden unexpected death in infancy (SUDI). This used to be called SIDS or cot death.
- Baby's own bed: Put your baby in his or her own bassinet, cot or other baby bed. This keeps them free from other adults or children who might smother and accidentally suffocate them. The bed should be firm and flat, free from gaps that could trap or wedge your baby and free from objects that might cover their face or head (no pillows, toys, loose bedding, or bassinet/cot bumpers). Wedges and positioning devices are not recommended.
- Sleeping position: Put your baby down to sleep on their back. Make sure your baby's feet are near the bottom of the bed so there is no wriggling down under blankets.
- Room sharing: Put your baby to sleep in a cot or bassinet near your bed while you sleep for the first 6 months. Make sure at least one parent is alert to your baby's needs and free from alcohol or drugs.
- Avoid bed sharing or falling asleep with baby to prevent suffocation: If you choose to sleep in bed with your baby - give them their own sleep space (Pepi-pod, wahakura, moses basket).
- A smokefree baby, breastfeeding and immunisation also reduce your baby's risk of SUDI.
If you need financial help so that baby can have his or her own bed you may be eligible for a grant from Work and Income. Depending on your situation, you may or may not be required to pay back the grant.
Registering your baby’s birth
The hospital (or your LMC if you had your baby at home) has to notify the Registrar of Births within five working days of your baby’s birth. The hospital will also give you a copy of the birth registration form for you to complete.
It is compulsory for you to complete and return this form to Births, Deaths and Marriages Central Registry, PO Box 10526, Wellington 6143, as soon as possible after the birth.
Start of your Well Child visits
Your final mother and baby check usually occurs between four and six weeks after your baby’s birth. This marks the end of your maternity care. Up until six weeks, you are still able to contact your LMC about any maternity-related problem.
You and your child have the right to publicly funded Well Child Tamariki Ora care. This Well Child care is different from the medical care you receive when your child is ill.
Talk to your LMC about who provides Well Child services locally. Some examples of Well Child providers are Plunket, the general practice team (but they may charge a co-payment), some Māori and Pacific providers, or the public health service. If you want your baby to have Well Child care, your LMC will refer you to your Well Child provider, usually between four and six weeks after your baby’s birth.
At six weeks, you can also take your baby to your usual GP for a further check. This is the same time as a baby’s first immunisation is due. This check is not a maternity visit or a Well Child visit but is part of the subsidised primary health care for children from birth to six years. You may be charged a part-payment for this.
Immunisation
Immunisation protects babies from twelve serious disease and begins when your baby is six weeks old. Immunising your baby at the recommended ages is the best protection against these diseases. The Ministry of Health supports immunisation but it is your choice whether to immunise your baby. All childhood immunisations are free in New Zealand. For more information talk to your health professional, contact the Immunisation Advisory Centre on 0800 IMMUNE (080 466 863) or visit the Ministry of Health website.
Returning to work
If you are returning to work and your baby will be using childcare facilities, try to make arrangements that allow you to easily see your baby during work time so you can continue breastfeeding. If you can’t do this, you can give your baby expressed breast milk while you are at work and breastfeed at other times of the day. One breastfeed a day is enough to continue lactation. Your LMC can advise you how to sterilise containers and safely store expressed breast milk in the fridge or freezer.
Appendices
Further information for pregnant women
Ask your LMC or Well Child provider for Ministry of Health pamphlets. You can order free copies from your local public health service or through the website www.healthed.govt.nz, which has the latest list of resources. Women who are pregnant or have just had a baby will be especially interested in the information in the pamphlets on the folllowing topics (the pamphlet codes are in brackets):
- alcohol (HE2523)
- breastfeeding (HE2098)
- SUDI/SIDS (HE1228)
- folic acid and spina bifida/iodine and iodine deficiency (HE4147)
- healthy eating and being active during pregnancy (HE1805) and while breastfeeding (HE1806)
- hepatitis B and C (HE4182)
- immunisation (HE1323)
- infant formula (HE1306)
- listeria (HE9007)
- antenatal HIV screening (HE1832)
- screening and testing for Down syndrome and other conditions (HE2382)
- newborn baby’s blood tests (HE2310)
- newborn hearing screening (HE2429)
- quitting smoking (HE10106)
- rubella (HE4172)
- sexually transmitted infections (HE7002)
- smokefree homes (HE1802)
- soy-based infant formula (HE1306)
- tuberculosis (TB) (HE2205).
You could also ask your LMC about additional information that may be available from other organisations in your area. For example, from:
- Home Birth Association
- La Leche League New Zealand
- NZ College of Midwives
- Maternity Services Consumer Council
- Parents Centre New Zealand.
You can also find further information regarding maternity services on the Ministry of Health’s website, and about screening for you and your baby on the National Screening Unit's website.
Choosing an LMC
Possible questions to ask before registering with an LMC are:
- Will you provide all my care, or will others be involved?
- How can I contact you if I need help or advice in and out of normal working hours?
- Are you taking leave in the month or months before or after my baby is due?
- Who will provide backup care for me if you can’t be there?
- What options do you offer for place of birth (eg, hospital, maternity unit, birthing unit, home birth)?
- Where will my antenatal visits be? In my home? At a clinic?
- How many antenatal visits can I expect to have? Will you visit me at home in early labour?
- What happens if you are away or with someone else when I go into labour?
- Will I be able to meet your backup midwife or doctor?
- What happens if I need specialist care during my pregnancy or my labour? If this happens, will you continue to provide care for me?
- If I stay in hospital, what will your role be?
- How many postnatal visits can I expect, both in hospital and at home?
- How many weeks do you visit for after the birth?
- Between visits, are you available for me to phone you for advice? Do you give me a chance to provide feedback on the care you provide?
You may also like to ask questions about your LMC’s experience and practice of delivering babies, such as:
- How would you describe the maternity care that you provide in pregnancy, labour and birth?
- What is your philosophy about childbirth?
- About how many births a year do you attend?
- How many other women have you got booked who are due about the same time as me?
- Have you had a standards review or an audit by your professional body?
If your LMC is a GP or a private obstetrician, other questions to ask are:
- Who will provide my midwifery care during labour?
- Can I meet the midwife who will provide me with care during labour?
- Who will provide my home visits when I go home from hospital?
Important contacts
| MUM 2 BE | Information on how to access maternity services and what you are entitled to receive | 0800 686 223 |
| Work and Income | Information on whether you qualify for financial help | 0800 559 009 |
| Inland Revenue Department (IRD) | Information on family assistance and parental tax credits | 0800 227 773 |
| Department of Labour | Information on parental leave | 0800 800 863 |
| Quitline (Quit - Me Mutu) | Advice on giving up smoking | 0800 778 778 |
| Healthline | Advice about your baby | 0800 611 116 |
| Health and Disability Commissioner | Help with complaints about the care you received | 0800 112 233 |
Complaints
If you have a complaint about the maternity care you have received, consider talking or writing directly to the person or organisation that provided the service. If your LMC was a midwife then you can download a feedback form from www.midwife.org.nz or contact 03 377 2732 for local resolution committee information. If you don’t feel comfortable about doing this, you can get support from an independent health and disability advocate, who is trained to help. There is no charge for this service. Your local advocacy service and the Health and Disability Commissioner can be reached by phoning 0800 112 233.
ISBN 978-0-478-41109-6 (print)
ISBN 978-0-478-41110-2 (online)
[HE1420]